Glucose is a major source of energy for the body and almost every cell in our bodies utilize glucose for energy. We obtain glucose from our diet, and usually, our blood glucose levels are tightly controlled. Insulin is the key regulator hormone for this control, and it acts on cells to promote movement of glucose from the blood into the cells. Glucagon is a second key hormone in glucose metabolism and effectively counters the effects of insulin. Both hormones act on the liver, muscles, and adipose tissue (1).
It is important that we maintain our glucose levels within a healthy range. If our glucose levels are too low (<3.9mmol/L) we experience hypoglycemia and symptoms can range from irritability and shakiness to loss of consciousness and seizures. High blood glucose levels can affect our concentration, increase thirst, cause frequent urination, lead to headaches, light-headedness, nausea, and fatigue. We should all therefore aim to maintain our blood glucose levels within a healthy range as irregular or extreme levels can lead to more serious conditions (1).
Being able to manage our blood glucose levels effectively, requires the ability to measure and track our glucose levels. Most tests however require the analysis of blood, and these tests include the measurement of fasting glucose levels, an oral glucose tolerance test, and/or the measurement of glycosylated haemoglobin, also known as HbA1c (1).
Measuring our fasting glucose levels or assessing the glucose response after eating are good analytical methods to evaluate whether your blood glucose levels are healthy. If a person’s fasted levels are higher than normal, they have what is called impaired fasting glucose (IFG). The blood glucose response after consuming glucose can also indicate whether your blood glucose levels are healthy. If your glucose levels are above 7.8mmol/L two hours after consuming glucose, you have what is called impaired glucose tolerance (IGT). Both IGT and IFG are considered prediabetic states (1,2). A final measure is HbA1c. Glucose in our blood binds to proteins, carbohydrates and fats, and the degree of glycosylation is proportional to your average blood glucose as the binding of glucose to haemoglobin is irreversible. Red blood cells have a lifespan of 10-12 weeks and so HbA1c shows your average glucose levels over the previous three months, and so is a reliable, and the gold-standard diagnostic measure (1).
Technology ushering in a new era of glucose monitoring
Continuous glucose monitors (CGMs) continually measure the blood glucose levels and give real-time updates. They measure glucose levels through a painless micro-needle in a button-sized transmitter that sends the data to a receiver or smartphone. The transmitter stays in place for 1-2 weeks and you can swim/shower etc. with it. Some CGMs are now implantable and stay in place for 3 months and they are able to provide detailed insights into a person’s blood glucose levels, and with it, new assessment metrics.
Time-in-Range (TIR) is one of these new metrics. Time-in-Range (TIR) is the amount of time a person spends within a target blood glucose range: for healthy people this is between 3.9 and 7.8mmol/L. It requires CGM monitoring, and it measures glucose excursions throughout the day (3).
Excursions are most noticeable after eating and are referred to as postprandial glucose (PPG). It is these post-prandial excursions that we need to be most attentive too as large clinical trials and systematic reviews have shown that the biggest risk factors arising out of unhealthy glucose levels are attributable to PPG, not our fasting glucose levels. PPG excursions increase our risk of heart disease, stroke, atherosclerosis, blindness, kidney disease, neuropathies. Many people incorrectly believe that these risks are only for diabetics, but the risk increases dramatically as blood glucose levels exceed the normal range (4,5).
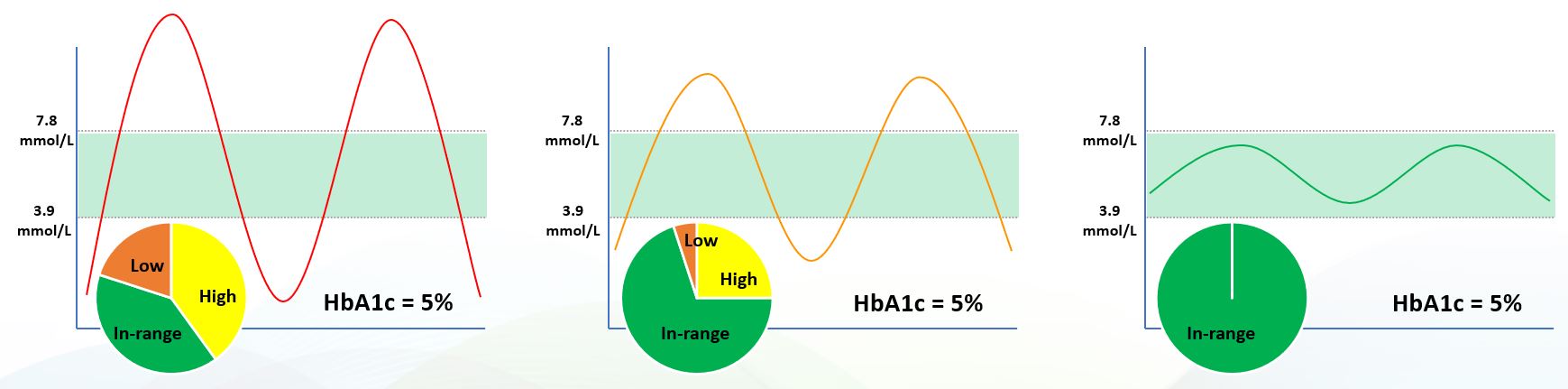
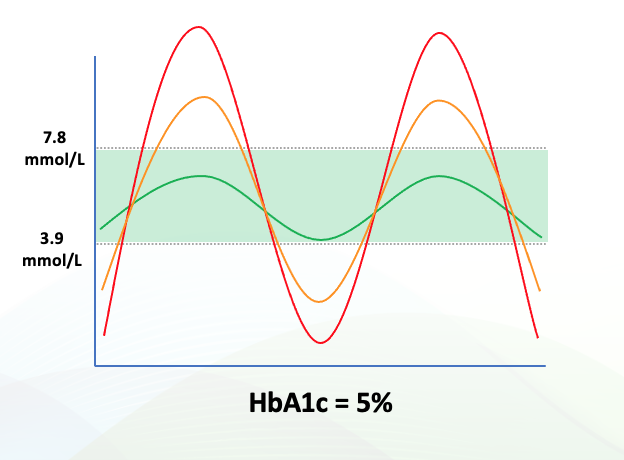
This is why TIR is such an important metric. Other measurements may give you an indication of whether your glucose levels are -on average- within the healthy range, but they don’t give you insights into optimizing your health. A comparison with HbA1c with TIR illustrates this point. In the three cases below, all three subjects have the same HbA1c value. They have very different Time-in-Range. The first subject has poorly controlled glucose levels, with dangerous highs and lows, and spends more time out of range than in range. The subject in the middle is meeting current guidelines but is still outside of the optimum range for 30% of the day, increasing her/his risk of oxidative damage to the sensitive tissues in the cardiovascular system, eyes, and kidneys. The subject on the right is optimized and spends 100% of her/his time within a tight and healthy blood glucose range. This is what everyone should strive for, and this is a benefit that an ingredient like Reducose® can deliver. It lowers the big peaks and eliminates the crashes in your blood glucose after eating, helping you to maintain healthy glucose levels throughout your day.